BACKGROUND
Myelodysplastic syndromes (MDS) are a heterogenous group of myeloid neoplasms. Patients may present with nonspecific signs and symptoms such as fatigue, infections, bleeding, and bruising. Bone marrow aspiration and biopsy are used to confirm diagnosis and are critical in the evaluation of bone marrow cell morphology and cellularity necessary for risk classification.
Patients stratified as higher-risk MDS (HR-MDS) have worse overall survival and a higher risk of transformation to acute myeloid leukemia (AML). Treatment of HR-MDS can be challenging. While hypomethylating agents azacitidine and decitabine are the only approved drugs for HR-MDS, there are clinical and translational studies for other treatment approaches. The only curative treatment at present is hematopoietic stem cell transplantation (HSCT), for which only a portion of patients may qualify.
This study sought to identify potential missed opportunities in care, including time to diagnosis (Dx) and treatment, by evaluating differences based on underlying sociodemographic and clinical characteristics of newly diagnosed patients with HR-MDS.
METHODS
This is a retrospective cohort study of commercial and Medicare Advantage health plan members with evidence of newly diagnosed HR-MDS in the Optum Research Database (ORD). Additional Optum datasets were linked to the standard ORD to allow for the inclusion of additional socioeconomic (SES) and social determinants of health (SDoH) variables. The study period was 1 January 2016 to 31 July 2022. Adults with ≥1 inpatient claim for HR-MDS or ≥2 outpatient claims for either MDS or HR-MDS (requiring at least 1 to be HR-MDS) on 2 separate dates between 1 January 2017 and 30 April 2022 were eligible for inclusion. The earliest HR-MDS claim was the index date. A period of 12 months prior to the index date was used to assess baseline characteristics. Patients were followed for at least 3 months post-index until the earliest of AML Dx, death, end of continuous enrollment, or end of the study period.
RESULTS
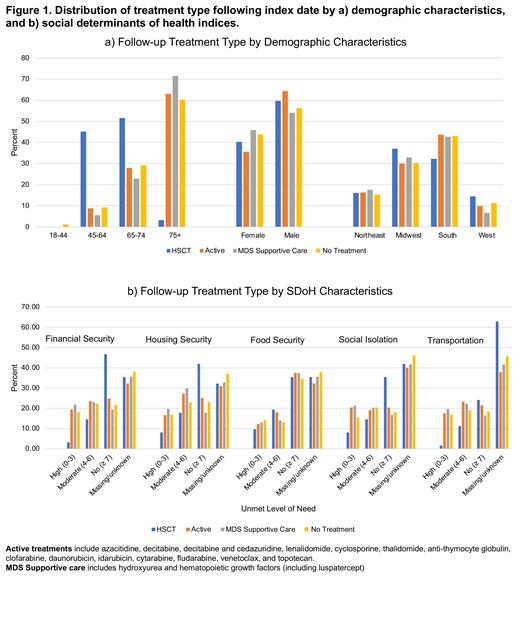
The study criteria were met by 1710 patients. Median age at HR-MDS Dx was 77 years, and 40% of patients had baseline Charlson comorbidity score ≥3; 22% had no claim for a bone marrow biopsy or aspiration in the 12 months prior to index or during variable follow-up. Patients were categorized hierarchically based on level of treatment received: HSCT occurred in 4% of patients, 33% had evidence of active treatment, 26% received MDS supportive treatment, and 37% had no treatment in the variable follow-up period. Patients who received HSCT had the lowest Charlson score (mean 1.3), followed by those who received active treatment (mean 2.2), no treatment (mean 2.3), and MDS supportive treatment (mean 2.8). Patients who received active treatment and those who received no treatment appeared to have a similar average age (76 years), similarities in baseline comorbidities (autoimmune conditions, diabetes, and hepatic and renal diseases), and similarities in underlying SDoH and SES characteristics. Male patients made up 58% of the total study population; the prevalence by sex varied within treatment groups where male patients were 64% of the active treatment group but only 54% of the MDS supportive treatment group (Fig. 1a). HSCT patients had the least likelihood of unmet SDoH need, whereas those in MDS supportive care generally had the lowest chance of no unmet need (Fig. 1b). Few patients (7%) had claims indicative of clinical trial participation after index; clinical trial participants were healthier (mean Charlson score 1.9 vs 2.4) and younger (only 37% were aged 75+ vs 64% of non-participants in this age group). Patients not participating in clinical trials were more likely to have unmet financial or housing security and transportation access challenges. White and Asian patients had the highest rates of whole blood transfusions (5.4 and 5.7 per 100 person-months, respectively), while Hispanic patients had the lowest rate (2.5 per 100 person-months).
CONCLUSION
A large proportion of HR-MDS patients had no evidence of active treatment during the variable follow-up. HSCT and clinical trial participation were low in the study; these patients were younger, had fewer comorbidities, and did not experience financial, housing, or transportation issues. To ensure guideline concordant care, there is a need to further contextualize drivers of treatment in clinical practice, including patients' preferences.
Disclosures
Moore:Optum: Current Employment, Current equity holder in publicly-traded company. Engel-Nitz:Optum: Current Employment, Current equity holder in publicly-traded company; Daiichi Sankyo, Inc.: Other: Research funding to Optum; Gilead: Other: Research funding to Optum; AstraZeneca: Other: Research funding to Optum; Kite Pharmaceuticals: Other: Research funding to Optum; Pfizer: Other: Research funding to Optum; Takeda: Other: Research funding to Optum; Novartis: Other: Resarch funding to Optum; Exact Sciences: Other: Research funding to Optum; GlaxoSmithKline: Other: Research funding to Optum. McMahon:Gilead Sciences, Inc.: Current Employment. Beal:Gilead Sciences, Inc.: Current Employment, Other: Restricted Stock. Jhaveri:Gilead Sciences, Inc.: Current Employment, Other: Stock or other ownership. Williamson:Amgen Inc.: Current equity holder in publicly-traded company; F. Hoffmann-La Roche AG: Current equity holder in publicly-traded company; Gilead Sciences, Inc.: Current Employment, Current equity holder in publicly-traded company. Andrade:Optum: Current Employment, Current equity holder in publicly-traded company. Landis:Optum: Current Employment. Sadek:Gilead Sciences, Inc.: Current Employment. Hogea:Gilead Sciences, Inc.: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal